A team of UCLA researchers from the schools of engineering and medicine successfully correlated images of surgical flap edema in rat models to evaluate the potential of terahertz imaging to accurately predict surgical flap viability during healing.
Currently, clinicians must keep patients under constant, postoperative surveillance to see if surgically-created skin flaps are healing properly. The successful development of an imaging technique that can identify compromised flaps earlier than visual inspection could mitigate infection rates, scarring, and patient cost.
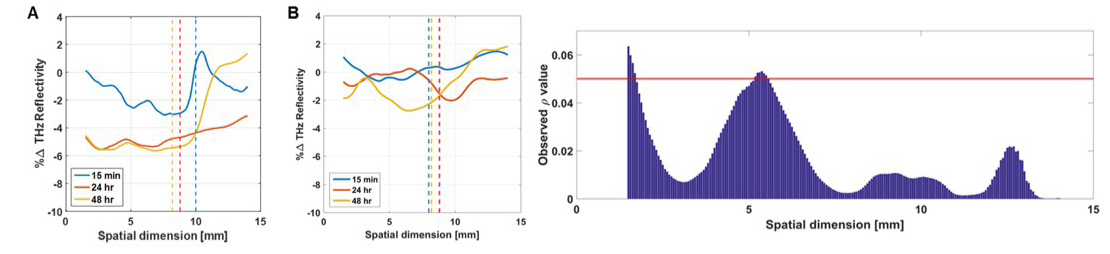
The research team recently completed a set of trials on rats, which have similar skin composition to humans. They found that viable and unviable skin grafts could be distinguished from each other as early as 24 hours after the initial grafting. The research required close collaboration from many departments across UCLA, including Electrical Engineering, Bioengineering, General Surgery, Head and Neck Surgery, Radiology, and Pathology.
Zach Taylor, an assistant professor with appointments in Bioengineering, Electrical Engineering, and Surgery, and a senior author on the published work, said the research team grew at every step of the research process as expertise was needed from different fields.
The team’s establishment would not have been possible without co-senior author Professor Maie St. John, the Samuel and Della Pearlman Chair in Head and Neck Surgery and co-director of the UCLA Head and Neck Cancer Program, Professor Taylor said.
While there is some debate about terahertz imaging’s abilities, Professor Taylor said the community has found it to be very sensitive to water, and mostly insensitive to everything else. The team ultimately focused on wounds because tissue water content – or edema – varies significantly following injury or surgery.
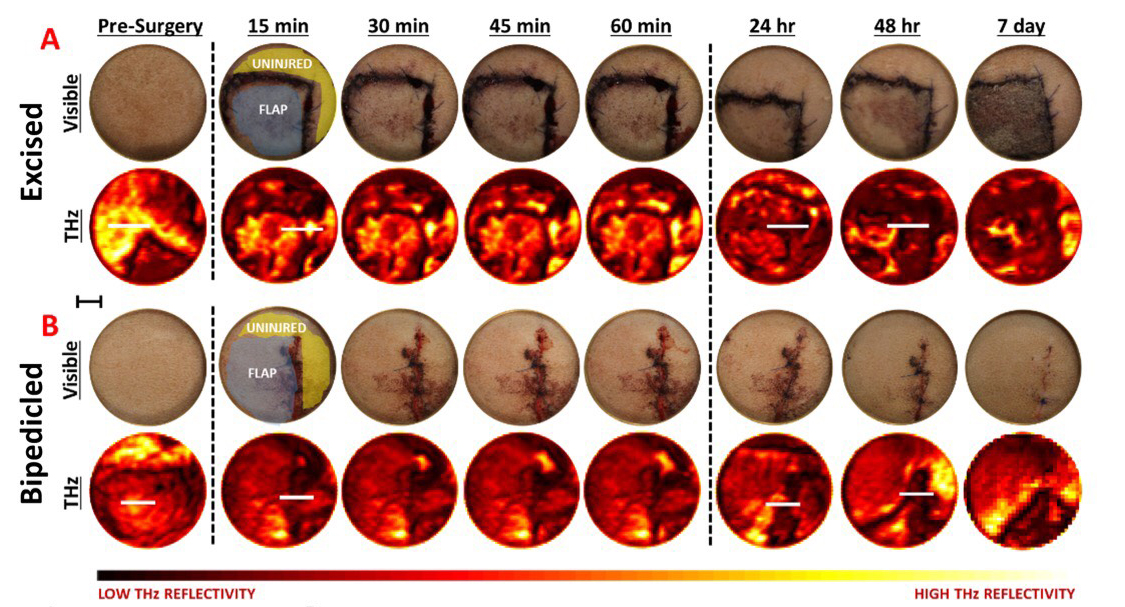
Across time, patterns in tissue water content variation in surface tissue correlates with wound which changes when tissue experiences swelling or an edema, can indicate how a wound is healing.
The basis for the technology driving the surgical flap imaging system was developed decades ago for radio astronomy. More recently, research and applications have broadened to high speed communications, nondestructive evaluation, and medical diagnostics. The ThZ frequency is unique because it combines traditional imaging with radio frequency engineering.
The ThZ images of surgical flaps show contrast between different levels of water concentration in the examined tissue, enabling clinicians to see where the skin is improperly hydrated and predict tissue death earlier. Traditional methods of observation are limited to the visible appearance of tissue and assessment by a trained doctor is typically too slow to prevent tissue death. Quantitative methods are mostly based on imaging the presence of blood in the tissue, but fluid build-up can obscure the quantification of blood flow and limit clinicians’ ability to identify compromised tissues.
Professor Taylor originally worked in ThZ security imaging before applying his research to diagnostic medical imaging applications. Collaborating with clinicians was essential to develop practical applications for terahertz imaging that directly improved doctors’ ability to help patients.
“You can work on medical imaging research on your own, but if you don’t engage clinicians you’ll never know the potential utility or value of the work,” Professor Taylor said. “Projecting your data onto the known physiology is a big challenge and, in the case of surgical flap viability, you need people who are experts on the inflammatory response related to surgery,” he added.
While Professor Taylor is excited by these results, the team faces a unique challenge working at UCLA.
“It’s humorous that we developed this research program here since UCLA plastics surgeons are so good the surgical flap failure rate is zero. There is, however, a non-trivial failure rate outside of UCLA and we are working hard to meet this need.”